The LIVING Trial is a lifestyle intervention program aimed at preventing type 2 diabetes mellitus among South Asian women with a prior history of had gestational diabetes mellitus.
The primary goal of the LIVING trial was to assess whether a culturally appropriate lifestyle intervention program tailored to the SA context, offered to women after gestational diabetes (GDM), could reduce the incidence of type 2 diabetes. This intervention aimed to be affordable, acceptable, and scalable.
Funding for the project was provided by the National Health and Medical Research Council of Australia (NHMRC) Global Alliance for Chronic Diseases (GACD) Grant (APP1093171) and the Indian Council of Medical Research (ICMR) GACD Grant through the All India Institute of Medical Sciences, New Delhi.
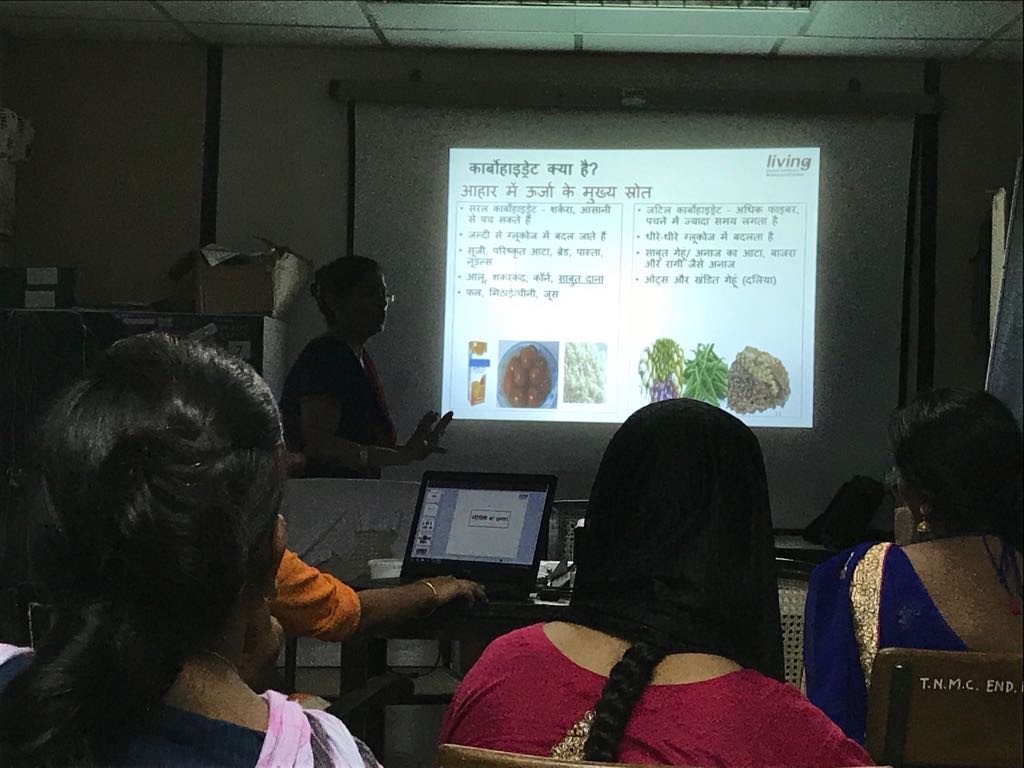
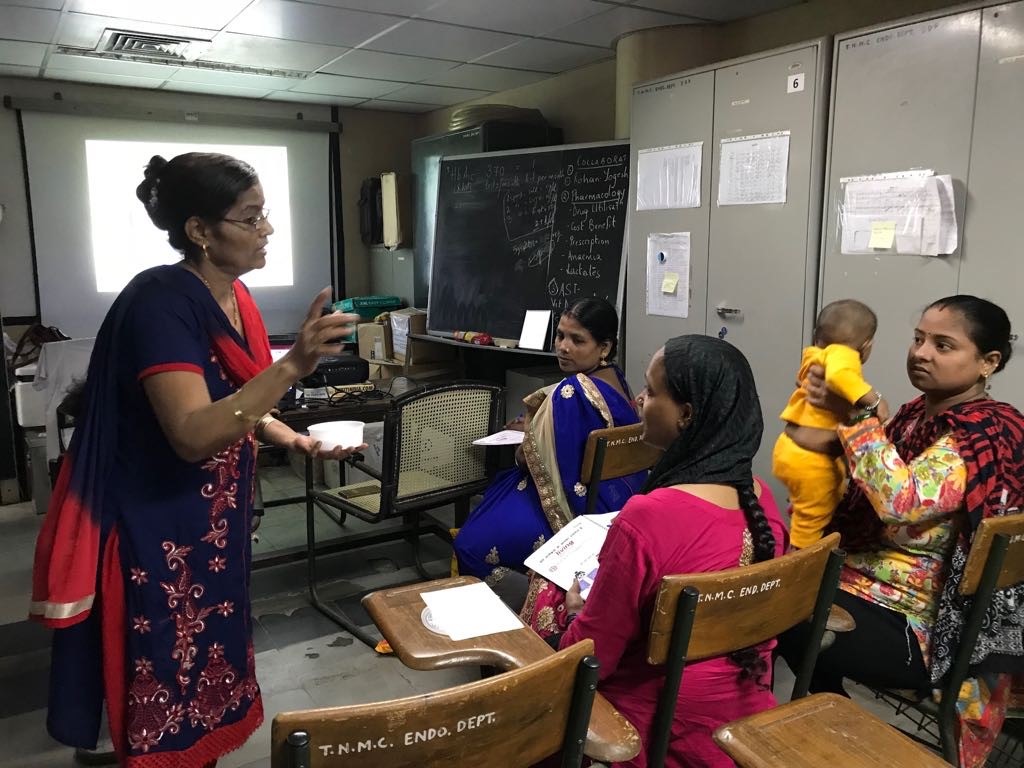
The LIVING TRIAL was an open-label parallel-group pragmatic individual randomised controlled trial with blinded primary endpoint adjudication. Participants from hospitals in India, Bangladesh, and Sri Lanka were randomized to either the intervention or control arm and be followed up for three years. The intervention comprised of a low-intensity lifestyle modification program focused on diet and physical activity delivered as four face-to-face group sessions combined with remote on-going support, and an intensification offering when needed.
New Delhi
Delhi & Hyderabad
Dhaka, Bangladesh
Kelaniya, Sri Lanka
Sydney, Australia
Melbourne, Australia
Women with recent GDM have increased risk of developing type 2 diabetes. This trial investigated a 12-month lifestyle intervention vs usual care at 19 urban hospitals in India, Sri Lanka, and Bangladesh.
A total of 1823 women were followed up post-partum for an assessment of diabetes status. Among them, 1601 were randomised (800 to intervention group). Among the 800 participants in the intervention, 644 women (80.5%) received all program content. The COVID-19 lockdowns did impact the delivery model. Among 644 participants, who engaged in all group sessions, 476 women [73.9%] received some or all content through individual engagement, and 315 women [48.9%] received some or all content remotely. No significant difference was found between the two groups in worsening of glycaemic status. However, this study did find that a large proportion of women in South Asian urban settings developed dysglycemia soon after a GDM-affected pregnancy. The findings suggest that alternate or additional approaches are needed, especially among high-risk individuals.

CCDC envisions to reduce chronic disease burden and promote innovative science that has the potential to improve human health through implementation and translational research.
Institutional Ethics Committee
Department of Health Research (DHR) Registration Number: EC/NEW/INST/2024/4768
Office of Human Research Protections (OHRP) FWA No: FWA00012746
Centre for Chronic Disease Control © 2025 All rights reserved.